Order before 4pm and select Express Courier Delivery for Next Working Day Delivery
Pressure Ulcers or Bed Sores – The Cost and Prevention
Also known as pressure sores or bedsores, pressure ulcers are injuries to the skin and underlying tissue. These are primarily caused by prolonged pressure on the skin and can happen to anyone, but usually affect people confined to bed or sitting profile for prolonged long periods of time.
This may be the result of a number of medical conditions such as obesity, paralysis, conditions that affect blood supply i.e., diabetes or kidney failure or simply old age – people over 70 are more prone to have mobility problems and skin that is susceptible to damage.
Stages of Pressure Sores
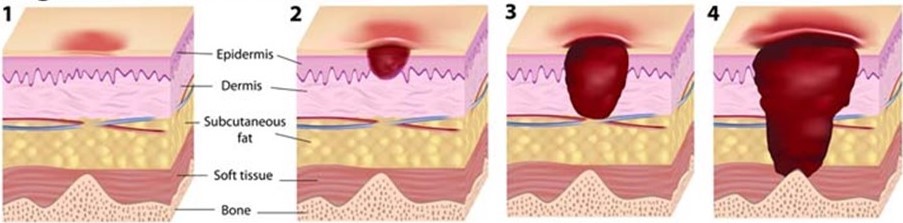
Pressure sores stages are now referred to as categories and these range from a category 1 to a category 4 – the most severe.
To help with getting it right, in the identification and categorising of your patients pressure sores, we have included a helpful and illustrative clinical review download from Wound Essentials.
The Cost
Perhaps most importantly, is the physical and mental cost of pressure ulcers to the patient. Patients developing pressure ulcers become extremely uncomfortable with these painful wounds and in turn this can cause further issues such as interfering with the patients sleeping. This domino effect from pressure ulcers then hampers recovery time and, in severe cases; can result in major harm or death.
The National Library of Medicine stated from a report in 2004 that in the UK, treating pressure ulcers cost the NHS more than £1.4 million every day!
Whilst this amount is staggering, and many resource articles today still go by that figure, following a revised definition and measurement summary in 2018 the actual figure (still back then) had risen to an eye-watering £3.8million every day!
Why is the financial cost so astronomical?
Overall, the vast proportion of costs in pressure sores treatment, are attributed to the healthcare professional – nursing costs. Just a relatively small amount is spent on bed sores treatment and specialist equipment. This is due to the care and treatment of pressure sores been an intensely ‘hands-on’ job for the nursing staff, with the patient having to be physically repositioned by up to four nurses every 15minutes!
Pressure Ulcer Prevention
Often attributed to the Dutch philosopher Desiderius Erasmus in around 1500, “Prevention is better than cure” is now a fundamental principle of modern health care and essential within health.
So, what steps to do we take to identify the risk?
We have touched briefly on those ‘at risk’ and now we can assist in the process of determining such individuals before they succumb to such medical implications. There are many professional sites available to assist on this topic such as:
- NICE (National Institute for Healthcare & Excellence)
- Stop the Pressure which provides details of many pressure reduction and pressure prevention initiatives across England
- The National Wound Care Strategy provides a helpful PowerPoint poster
- Developed in the 1960s, the Norton Scale is widely used to assess the risk for pressure ulcer in adult patients
Our initial mindset should be that all patients have the potential risk of developing a pressure ulcer and protocol should require an individual risk assessment for all patients, to enable a plan, implementation, and a prevention measure evaluation. To help with this process and ensure we are keeping to an approved system, frameworks such as the SKINN bundle updated to aSSKINg (as below image) help keep us to a recognised curriculum.
Download this helpful guide from SCIE & NICE Helping to prevent pressure ulcers
Berwick Care have been providing specialist equipment and consumables to care homes for over 25 years, and have a comprehensive knowledge of pressure relief mattresses, pumps, cushions and chairs. Browse our range of pressure relief products.

